Immunizations
You must E-Mail your immunization records and consent in PDF form before you are eligible to be booked for an immunization review with a Registered Nurse. Please try to send all required immunization documentation within 2 weeks or receiving your acceptance letter to student.wellness@usask.ca.
To ensure you complete your requirements on time please submit your documentation early. The Student Wellness Centre will contact you to book an appointment once your records are reviewed. Please be patient as the nursing staff is managing immunization records for all health science colleges.
All students in health science programs are required to have an immunization record completed and up to date to submit to their college. Completion of these requirements is mandatory for you to be able to do your clinical placements.
Health Science Colleges include:
Medicine, Physician Assistant, Nursing, Nurse Practitioner, Physical Therapy, Occupational Therapy, Speech-Language Pathology, all Dental Health Programs, Pharmacy, Nutrition, Masters of Public Health and Veterinary Medicine.
We ask that all Health Science students locate their childhood and adult immunization records. If your records are not in English please have them translated prior to submitting.
During your first visit for immunization review we will disscuss your college requirements and provide a tuberculin skin test (TST) if needed. The college of Medicine is the only group that will require a 2 step TST.
Where can I find my immunization records?
You can find your immunization record on your provincial on-line health record. If you do not have access to this please check with your parents, Public Health in the area where you grew up in, or your Physician’s office. If your records are not located in Canada, check with any family that may be in your home country. If you immigrated to Canada as a child, Immigration Canada requires an immunization record signed from a Physician in your country. Ask your parents for this form. If you do not or cannot locate any records, you must start your immunizations over – this is costly and timely. Please make every effort to locate your records.
Completion of the immunization requirements is the responsibility of the student. This includes locating childhood and adult immunization records.
Medical Electives require an immunization review and completion of forms. There is a $30.00 charge for this service.
Your student health plan will provide coverage for up to $150.00 of vaccine every year.
Gardasil- As of April, 2025 ALL individuals are eligible to start to thier Publically funded Gardasil series prior to the age of 27. Publicly funded vaccine is not currently available at the Student Wellness Centre. Here is the link to Public Health.
If you do not meet the age requirements for publicly funded vaccine (over the age of 26), you can book with a Nurse Practitioner at the Student Wellness Centre and receive a prescription for the vaccine. (Gardasil Vaccine is a series of 3 doses, and costs approximately $180.00 per injection). If you are covered under the Student Health Plan your insurance covers $150.00 per calendar year for vaccines).
Tdap (Tetanus/diphtheria/pertussis)- Usually given every 10 years. Given at 26 weeks of pregnancy with each pregnancy. No charge for boosters
Hepatitis A – $60.00 for each injection- series of 2
Some individuals are eligible for publicly funded Hepatitis A vaccine through public health-talk to your health care provider.
Hepatitis B – Publicly funded if born after 1984
Twinrix (Hep A/Hep B combined) - Cost approximately $70 each - series of 3. A prescription is required for this vaccine.
Annual Flu & Covid Vaccine (October-March) – Information will be updated yearly in October.
We do not provide counseling on travel vaccine information (Public Health)
Annual Flu Vaccine administration will begin again in October 2025, and will run until March 2026.
Sexual Health
Who should have STI testing done? Anybody who is sexually active!
STI’s can be spread in the following ways:
- Unprotected vaginal, anal, and oral sex
- Skin to skin contact with an infected area
- Kissing an infected area
- Sharing sex toys
- Mother’s can share STI’s to their child during pregnancy, labor and breastfeeding
Sex is normal and it is a healthy part of life, so whether you are planning on becoming sexually active or already sexually active make sure you know the best way to keep yourself and your partners healthy and safe.
Young healthy adults are encouraged to complete a routine STI screen yearly and with each new partner. This typically includes a urine sample and/or swabs for chlamydia and gonorrhea and blood tests for HIV, Syphilis and Hepatitis C. However, if you are at higher risk for an STI, we recommend you have more frequent STI screens. Risk factors include multiple partners, unprotected sex, men who have sex with men (MSM) and a previous history of STI.
When you come into the Student Wellness Center for an STI screen, you can expect us to treat you with respect, keep your information confidential and provide you with support as you need. We will ask you some personal questions, this is to assess risk factors and will help us to make appropriate suggestions for you.
STI testing for Chlamydia and Gonorrhea is usually a simple urine sample; however Chlamydia and Gonorrhea can also be found in the rectum and throat. A throat and rectal swab can be completed to test for infection in these areas. You do not have to have symptoms in order to request STI testing.
As part of your STI screening your provider may suggest bloodwork to screen for HIV, Syphilis and Hepatitis C. This is routine screening.
All positive STI tests are required by public health to complete a confidential contact tracing form, this will be completed with a Registered Nurse.
Can I be tested for genital warts (HPV) and herpes (HSV 1 & HSV 2)?
Typically, genital warts and herpes are diagnosed during a physical assessment when you are symptomatic (this means when sores or lesions are present) by a Physician or Nurse Practitioner.
*If you would like an appointment for STI screening, please contact the Student Wellness Center (306) 966- 5768.
Additional Sexual Health Resources:
The Student Wellness Centre now has Take Home HIV testing Kits available.
Students are welcome to request a kit at anytime (you can take up to 5 at a time), just present to reception and ask to speak with a nurse.
Pre exposure prophylaxis for the prevention of HIV is a prescribed medication regimen to help reduce infection rates of HIV, it is free to Saskatchewan residents. PrEP is taken daily to help reduce your risk. If you are interested in PrEP or feel that you may be at risk for contracting HIV, please reach out to the SWC for an appointment. PrEP is not right for everyone, but we would be happy to discuss your options.
Some reasons to consider PrEP include:
PrEP is recommended for MSM and transgender women who report condomless anal sex and who have any of following additional risk factors:
- One or more HIV-positive sexual partner(s).
- Recent (within 6 months) sexually transmitted infection (STI)
- Multiple sex partners
- History of inconsistent or no condom use for anal intercourse
PrEP is not recommended in the context of a closed, stable relationship with single partner if there is a no risk of transmissible HIV.
Heterosexual men or women:
Because HIV prevalence in the general Canadian heterosexual population is low, recommendations are focused on persons in relationships where one partner is HIV positive and the other is HIV negative. If the HIV-positive partner has a significant risk of transmissible HIV and condomless vaginal or anal sex is also reported, then PrEP is recommended for the HIV-negative partner.
For people who use injection drugs, this will usually consist of:
- Sharing injection equipment
- Injecting once or more times per day outside of safe injection sites
- Repeated courses of non-occupational post-exposure prophylaxis (nPEP)
Additional resources for PrEP:
When choosing a method of contraception, protection againtst STI's should be considered. Although hormonal contraceptives and IUDs are highly effective at preventing pregnancy, they do not protect against STIs, including HIV. Consistent and correct use of the male condom reduces the risk for HIV infection and other STIs, including chlamydial, gonococcal, and trichomoniasis.
Long Acting Reversible Contraceptives:
Hormonal intrauterine device (IUD)—This IUD is a small T-shaped device placed inside the uterus by a qualified Healthcare Professional. It releases a small amount of progestin each day to keep you from getting pregnant. The hormonal IUD's we currently use include the Kyleena and the Mirena.
Copper T intrauterine device (IUD)—This is a non-hormonal IUD placed inside the uterus by a qualified Healthcare Professional.
Implant (Nexplanon) - This hormonal birth control is a small rod inserted under the skin of the upper arm (usually placed in non-dominant arm). This implant releases the hormone etonogestrel and is effective at preventing pregnancy for up to 3 years.
Short Acting Reversible Contraceptives:
Injection or “shot” (Depo-Provera)—Women get an injection of the hormone progestin every three months. This injection can be administered by a qualified Health Care Professional.
Combined oral contraceptives—Also called “the pill,” combined oral contraceptives contain the hormones estrogen and progestin.
Progestin only pill—Unlike the combined pill, the progestin-only pill (sometimes called the mini-pill) only has one hormone, progestin. It is taken at the same time each day. It may be a good option for women who can not take estrogen.
Evra Patch—This skin patch is worn on the lower abdomen, buttocks, or upper body (but not on the breasts). It releases hormones progestin and estrogen into the bloodstream. You put on a new patch once a week for three weeks. During the fourth week, you do not wear a patch, so you can have a menstrual period.
Hormonal vaginal contraceptg releases the hormones progestin and estrogen. You place the ring inside your vagina. You wear the ring for three weeks, take it out for the week you have your period, and then put in a new ring.
Barrier Methods
Male condom- Worn by the man, a male condom keeps sperm from getting into a womans body. Latex condoms, the most common type, help prevent pregnancy, HIV, and other STIs, as do the newer synthetic condoms. Do not use oil-based lubricants such as massage oils, baby oil, lotions, or petroleum jelly with latex condoms. They will weaken the condom, causing it to tear or break.
Female condom- Worn by the woman, the female condom helps keep sperm from getting into her body. It is packaged with a lubricant and is available at drug stores. It can be inserted up to eight hours before sexual intercourse. They may also help prevent STIs.
Permanent Methods of Birth Control
Female Sterilization—Tubal ligation or “tying tubes”— A woman can have her fallopian tubes tied (or closed) so that sperm and eggs cannot meet for fertilization. The procedure can be done in a hospital or in an outpatient surgical center. You can go home the same day of the surgery and resume your normal activities within a few days. This method is effective immediately.
Male Sterilization–Vasectomy—This operation is done to keep a man’s sperm from going to his penis, so his ejaculate never has any sperm in it that can fertilize an egg. The procedure is typically done at an outpatient surgical centes about 12 weeks. Another form of birth control should be used until the man’s sperm count has dropped to zero.
Resources for contraception
How can I prepare?
- Please arrive at least 15 minutes before your appointment with a full bladder. You will need to complete paperwork and provide a urine test.
- We encourage you to drink some water and eat a light meal or snack before you arrive at the clinic.
- Your doctor or nurse practitioner may suggest you take ibuprofen (Advil) or acetaminophen (Tylenol) before your appointment for your comfort.
- You may want to plan for a ride home following the insertion, you may feel mildly lightheaded and/or experience some cramping
How long will the procedure take?
- You will be in the doctor’s treatment room for approximately 30 minutes.
- The IUD insertion takes between 5-15 minutes
- You are welcome to remain lying down for a while following the insertion if you are feeling lightheaded or having some cramping.
How can I take care of myself after my IUD has been inserted?
- It is common to have some cramps and spotting after your IUD has been inserted, this may last 1-7 days
- A warm heating pad or hot water bottle placed over your lower abdomen may help with cramps
- You may find ibuprofen or acetaminophen helpful - use as directed on the bottle
- Avoid strenuous exercise for at least 24 hours after insertion
- Check for IUD strings once each month or as advised by your doctor.
When can I have sex?
- You should wait at least 24 hours after your IUD has been inserted.
- Do not use tampons or douche for at least 24 hours after insertion.
When will my IUD start to work?
- Copper IUD – immediately
- Hormonal IUD - immediately if inserted during your period, otherwise 7 days after insertion. It is recommended to use condoms for the first seven days.
When should I call the Doctor?
- If you can’t feel the string or you feel your IUD may have moved out of place
- You think you may be pregnant
- You are having heavier than normal period
- You are having a fever or chills not associated with a cold or flu or a severe headache
- You have a sharp pain in your belly or pelvis.
- You are having foul smelling or abnormal vaginal discharge.
- You are having pain during sex.
- If the strings are bothering you or your partner-they may need to be trimmed
Nexplanon
- Please arrive to your appointment 15 minutes early with a full bladder. You will also need to bring your Nexplanon device with you.
- You will experince minimal pain or bruising during and after your insertion.
- You will also have a bandage for 24 hours after insertion.
- Abstinence or a back-up method of contraception for 7 days after insertion is advised.
Your IUD or Nexplanon will not protect you against sexually transmitted infections
Sometimes unexpected or unplanned situations occur.
If you ever find yourself in a situation where you are concerned about becoming pregnant, you need to know you have some options.
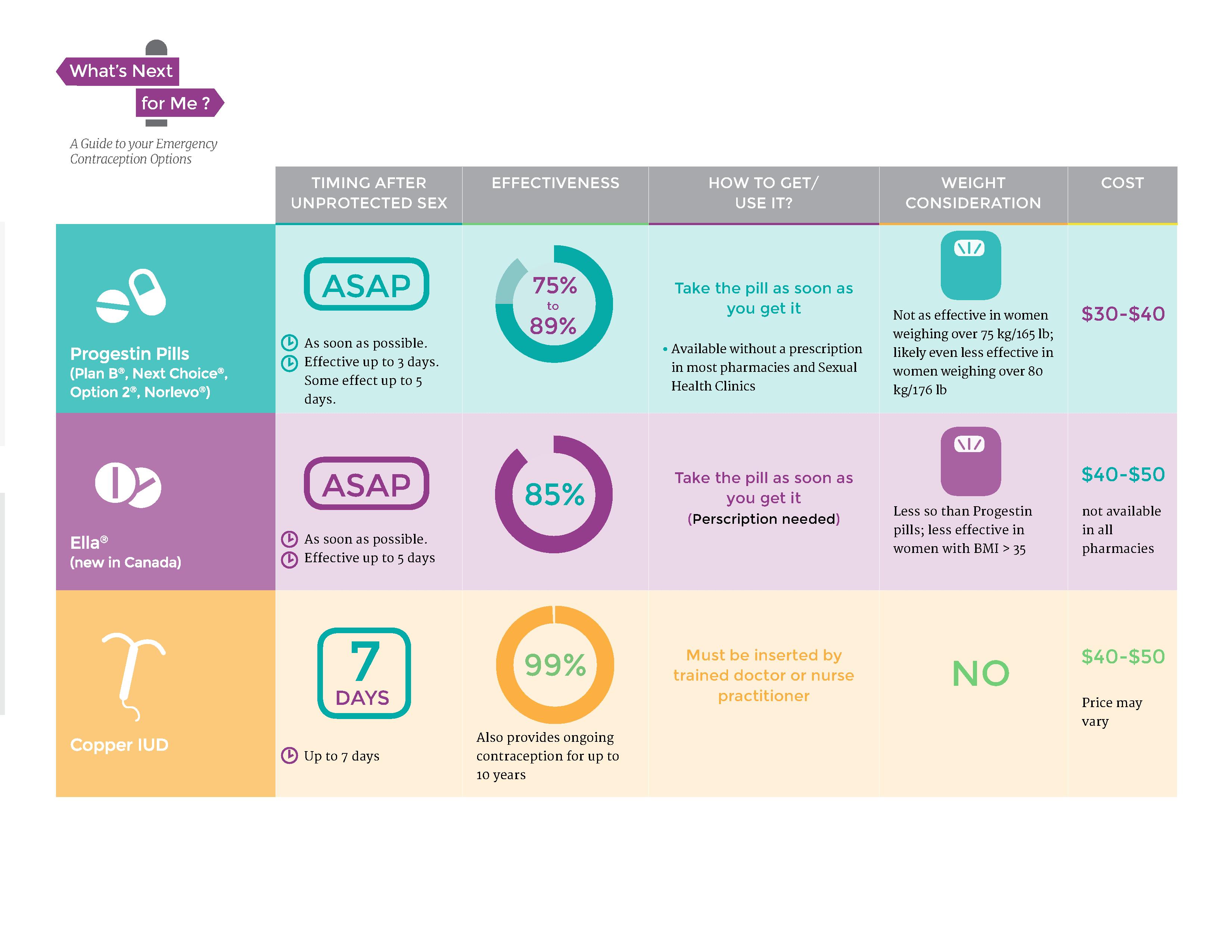
Emergency contraception can be used following unprotected intercourse or after protected intercourse where there was a failure of birth control method, for example a broken condom. There are two different options, these include the emergency contraceptive pill (morning after pill) and the copper IUD. The emergency contraceptive pill can be taken up to 72 hours after intercourse and is accessible from most pharmacies without a prescription. The copper IUD can be inserted up to 7 days following intercourse and will need to be placed by a qualified Healthcare Provider.
For some women pregnancy can be an exiting time, for others it may just not be the right time. It is ok to have several different feelings about your pregnancy and it is ok to learn about your options, whether it is parenting, adoption or abortion. In any circumstance the Student Wellness Center is here to provide you with support and help you manage over the course of your pregnancy.
If parenting is your choice, the health care providers at Student Wellness will be happy to assist you up to 26 weeks into your pregnancy and then will refer you on to an obstetrician. Following the birth of your child your health care provider will resume providing care for you and your child.
If you are seeking alternative options including termination or adoption you are welcome to come to Student Wellness for support and help with navigating your healthcare at this time.
In Saskatoon surgical abortion can be done up to 12 weeks, and medical abortion can be done up to 9 weeks. You must have a valid health card to cover your procedure and medications.
Referral can be made by a health care provider to a gynecologist for either medical or surgical abortion or self referral to the Saskatoon Community Clinic for medical abortion.
Adoption Support Center of SaskatchewanSafety & First Aid
Accidents happen, so we have provided you a list of commonly used materials that may be of help to you if you or someone you know has a minor injury. Please seek out medical care if you have a more serious wound, burn, break, or life-threatening emergency.
Wound Care
- Band Aids – various sizes
- Antiseptic solution for cleaning wounds
- Antibiotic ointment (ie, Polysporin)
- Adhesive tape
- Cotton balls
- Elastic bandage – 2-3” width
Medication (These medications are common and safe to use as directed. Please avoid these medications if you have had an allergy or adverse reaction to them in the past)
- For pain, fever, or headache – Ibuprofen (Advil) or Acetaminophen (Tylenol)
- For seasonal allergies or minor allergic reaction – an Antihistamine (Reactine, Claritin, Benadryl)
- For stomach upset or nausea - Gravol (Dimenhydrinate)
- For sore throat – lozenges
Other supplies to help you manage your minor emergencies
- Thermometer – digital
- Disposable hot/cold pack
- Cotton tip swabs
- Safety pins
- Tissue
- Tweezers
- Table salt-small container-for throat gargle or wound soak
- Hand sanitizer
Anyone who uses opioids, whether obtained by prescription or illegally, is at risk of an opioid overdose.
Know the signs of an opioid overdose:
- Trouble walking or talking
- Pinpoint pupils
- Shallow breathing
- Slow heartbeat
- Bluish, cold/clammy skin
- Seizures
Naloxone reverses the effects of an opioid overdose temporarily and will have no effect if opioids are not present. Naloxone is a safe medication, with few side effects.
It’s important to note that Naloxone treatment itself does not replace the need to seek immediate medical attention. Call 911 immediately if you suspect an overdose.
Take home naloxone kits can be obtained at the Student Wellness Center or Campus Pharmacy free of charge. If you are interested in having a naloxone kit, please contact the Student Wellness Center for information.
If you have or are interested in a take home naloxone kit, please look at this short video: Short video to watch
More information about Saskatchewan’s take home naloxone kits, opioid overdose and the Good Samaritan Act can be found at the following web address.
More information about opioidsNursing Procedures
Liquid nitrogen therapy, or cryotherapy, is a procedure to remove your wart by freezing it with liquid nitrogen. Cryotherapy may stimulate your immune system to fight viral warts. You may need to return to the Student Wellness Centre for repeat treatments every two weeks until the wart disappears.
What to Expect
-You may have pain and burning in the treated area for 1-3 days after your procedure.
-You may have redness and swelling to the area, or you may develop a blister. The blister may turn black in color. Do not try to remove the blister yourself. This could lead to infection and scarring.
-A scab may form in the treated area and will take approximately 1-2 weeks to fall off.
Aftercare
-Clean the area with soap and water as you normally would when showering.
-If the site is prone to irritation, you may cover with a bandage.
-If you are experiencing pain you may take Acetaminophen (Tylenol) or Ibuprofen (Advil). Follow the dosage recommendations on the bottle.
-If you start to experience signs of infection such as fever, redness, warmth or drainage to the site contact Student Wellness or another health care professional immediately for assessment.
-Repeat treatment every 2 weeks, or as instructed by your provider.
-Your provider may instruct you to exfoliate the callous covering your wart with a foot file/pumice stone prior to your next treatment.
Resources
UTI’s are a common concern in women of all ages.
Common symptoms include an urge to urinate (pee), burning with urination, urinating small amounts frequently, discomfort in pelvic area and strong smelling, cloudy or blood tinged urine. If you are having any of these symptoms, please call the SWC for an appointment.
Here are some tips to help decrease the risk of developing a UTI:
- Drink plenty of liquids, especially water. Drinking water helps dilute your urine and ensures that you'll urinate more frequently — allowing bacteria to be flushed from your urinary tract before an infection can begin.
- Drink cranberry juice. Although studies are not conclusive that cranberry juice prevents UTIs, it is likely not harmful.
- Wipe from front to back. Doing so after urinating and after a bowel movement helps prevent bacteria in the anal region from spreading to the vagina and urethra.
- Empty your bladder soon after intercourse. Also, drink a full glass of water to help flush bacteria.
- Avoid potentially irritating feminine products. Using deodorant sprays or other feminine products, such as douches and powders, in the genital area can irritate the urethra.
- Change your birth control method. Diaphragms, and spermicide-treated condoms can contribute to bacterial growth.
The nurses at the Student Wellness Center are happy to provide injections to students free of charge. The injections include but are not limited to:
- Depo-provera
- B12
- Gardasil
- Hormone Injections
- Allergy Shots
- Miscellaneous Immunizations
You must have a valid prescription from a Physician or Nurse Practitioner in order to receive your injection.
Earwax (cerumen) is produced in the ear canal. This wax traps dust and other small particles to prevent them from damaging or infecting the eardrum. Normally ears are self cleaning and this wax dries up and falls out of the ear canal on its own. Some people may produce more wax and or may have small ear canals causing excess wax to build up in the ear canal. Earwax can unknowingly be pushed deeper into the canal with the use of Q-tips, ear buds or ear plugs. This will cause the wax to become firm and block the ear canal (Earwax impaction).
Symptoms of earwax impaction include:
- Difficulty hearing
- Plugged, pressure or a “full” feeling in ears
- Ear discomfort or pain
- Ringing or itching in ears
How is earwax impaction diagnosed?
- Your health care provider will look in both of your ears with an instrument called an otoscope-this is painless
- If you require ear syringing, the nurses will provide you with additional instructions after consultation with a physician or nurse practitioner to confirm diagnosis.
Frequently Asked Questions
Do you see students on a walk-in basis?
Students who present for walk in services with a non-urgent concern may be asked to book an appointment and return at a later time. In order to reduce your wait time we encourage you to book an appointment when possible.
Some same day/walk-in appointments can be accomodated; however, we can not guarantee this. Please call the Student Wellness Clinic at 306-966-5768 for an appointment.
I am planning a vacation; can I get the appropriate travel vaccines at Student Wellness?
We recommend you make an appointment at the International Travel Center if you are planning a trip out of the country. For more information or to book an appointment visit:
Can I get a sick note at Student Wellness?
No, we do not provide sick notes for students. If you have missed a lab, class or exam please fill out STUDENT SELF DECLARATION OF ABSENCE found here: Declaration of absence
I don’t have a Saskatchewan Health Card; can I still access the Student Wellness Center?
Yes, however there may be a charge for your visit with a physician ($30.00) and if you require any lab tests (blood work/urine sample) you will incur a charge for this. You may be able to submit your receipts to your personal health insurance plan. If you would like to apply for a Saskatchewan Health Card please visit Apply for a health card
Contact Us & Emergency contacts
If you have a question for the nurses please reach out by email nurse.swc@usask.ca, we will monitor our email throughout the day. We will not provide medical advice but will do our best to assist with your concern and help you navigate the Student Wellness Center.
If you are wanting to book an appointment with your physician or with nursing, please call (306) 966- 5768.If you or someone you know is having an emergency, please call 911.
Call 811 (HealthLine) for non-emergency assistance
Family Medicine and Urgent Care Clinic on 8th Street
Poison Control Center - 1-866-454-1212
For emergency treatment advice for people exposed to all kinds of poisons including:
- Plants
- Drugs
- Mushrooms
- Pesticides
- Snake and spider bites
- Household cleaners and chemicals
This confidential service is available 24 hours a day, 7 days a week, all year round.
Mobile Crisis (24/7 access) – (306) 933-6200
Saskatoon Police Service – 76-25th Street East, Saskatoon
911 for emergency
Non-emergency call (306) 975-8300
RUH Emergency Department – 103 Hospital Drive, Saskatoon

